Case Study · Shared Vision
Digital Aftercare in Practice: Recovery Is a One Size Fits One
A 12-month, research-backed aftercare pathway that extends support beyond discharge — private, ethical, and human-centred.
“We saw people leave our care with good intentions — but once they went home, life took over. They needed a bridge between structure and independence.”
The Challenge
Structured support fades after discharge. Follow-up calls help, but they’re reactive and resource-intensive. People need private, ongoing guidance — especially in the first months.
Shared question: How might digital tools extend the therapeutic alliance rather than replace it?
The Vision
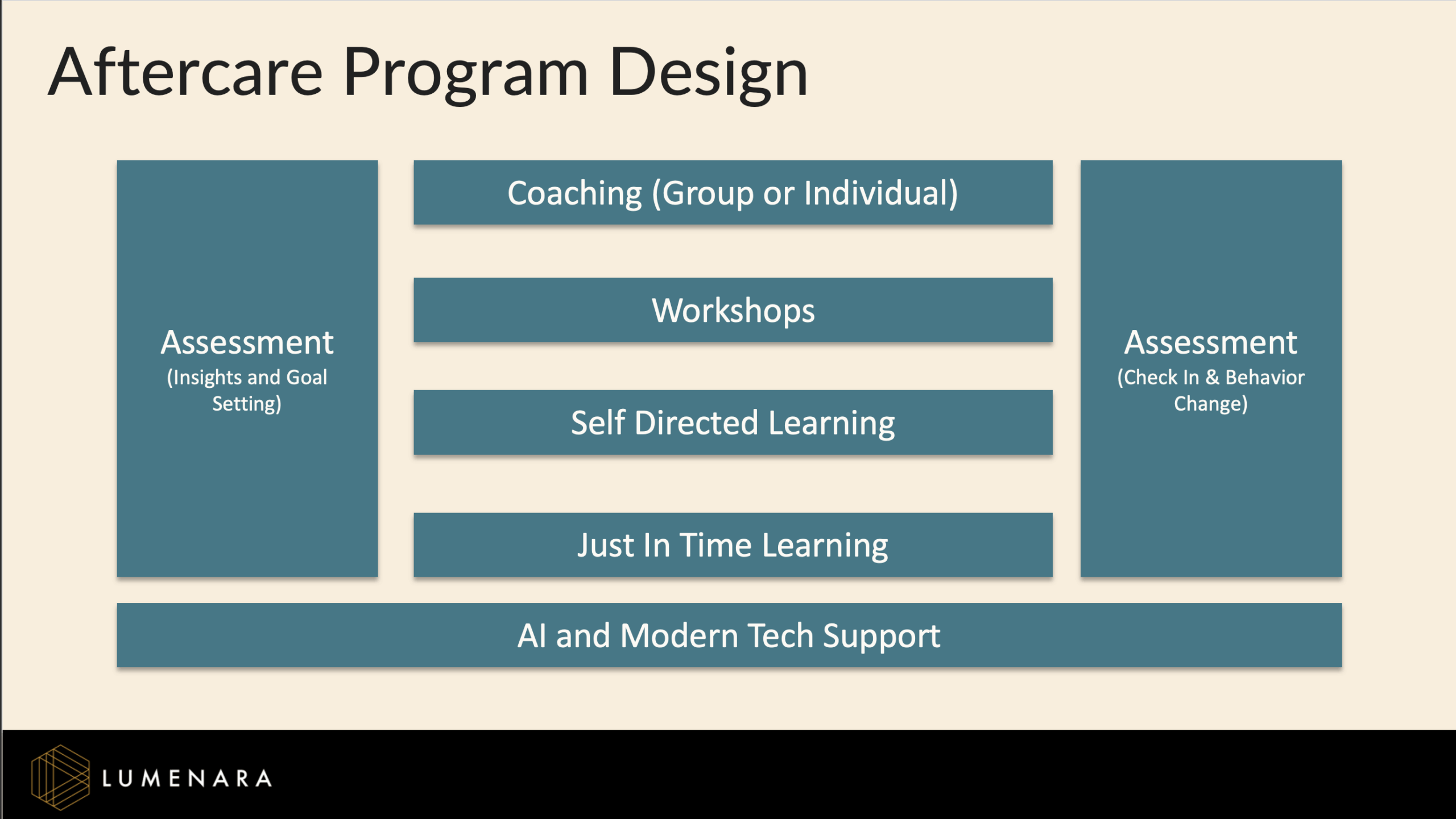
Together we designed a modern, evidence-based blended learning program that delivers remote support, anywhere and anytime via a 12-month digital aftercare pathway:
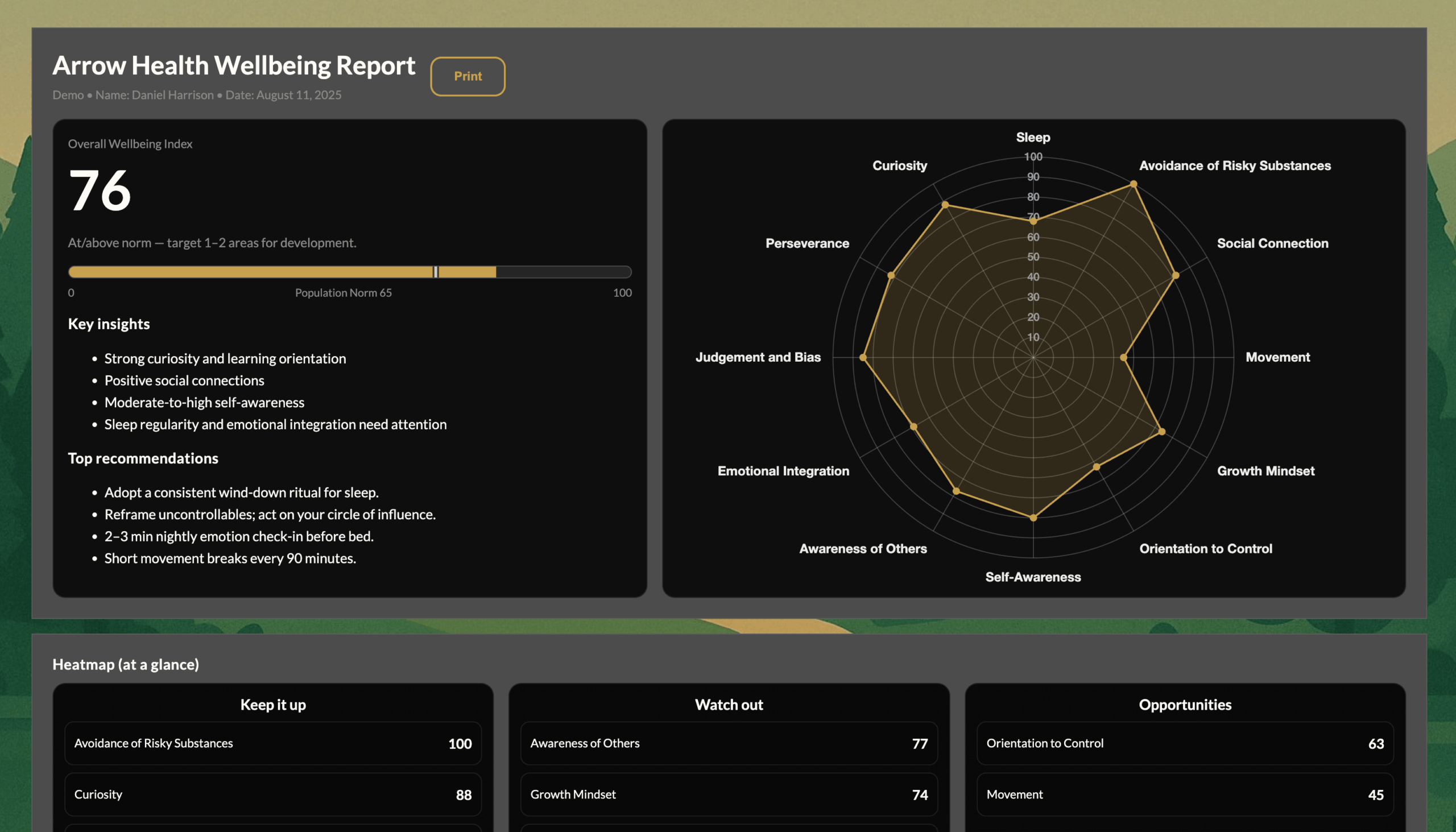
- SPARK “Living Well” Check-ins — brief assessments at 3, 6 and 12 months to track resilience and self-regulation.
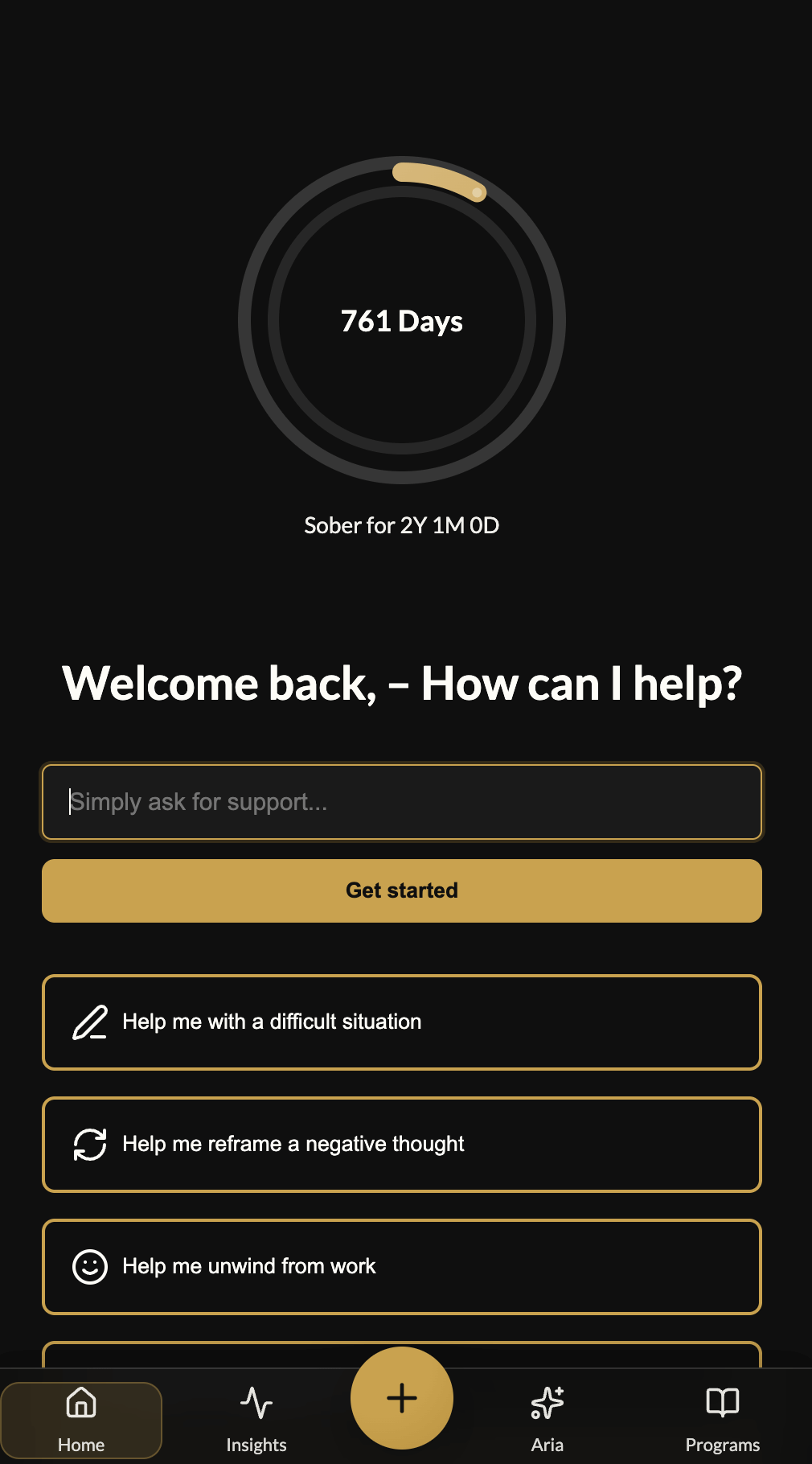
- Aria, the Reflective AI Facilitator — a private space for journaling and guided reflection that turns insight into practice.
- NeuroShift Micro-Practices — short, science-based activities that calm the nervous system and reconnect with values on demand.
- Blended Learning Program — modular, coach-supported sessions for onsite or remote participants.
“What struck us wasn’t just the tech — it was helping people stay connected to recovery long after discharge in a blended and intelligent way.”
The Potential Impact
- Maintain engagement through the high-risk 3–6-month window.
- Reduce relapse via timely nudges and reflective prompts.
- Give staff aggregated insights — never private journaling.
- Provide measurable outcomes for funders and accreditation.
Looking Forward
Recovery that travels with the person — powered by secure, ethical AI and adaptive learning — for individuals, families, and providers.
Request a Demo
Here the Full Case Study and See Lumenara in Action
Experience how our AI-enabled platform blends evidence-based psychology, modern design, and real-time support…